A Patient’s Guide to Hip Resurfacing
Forever Active
- Hip Resurfacing
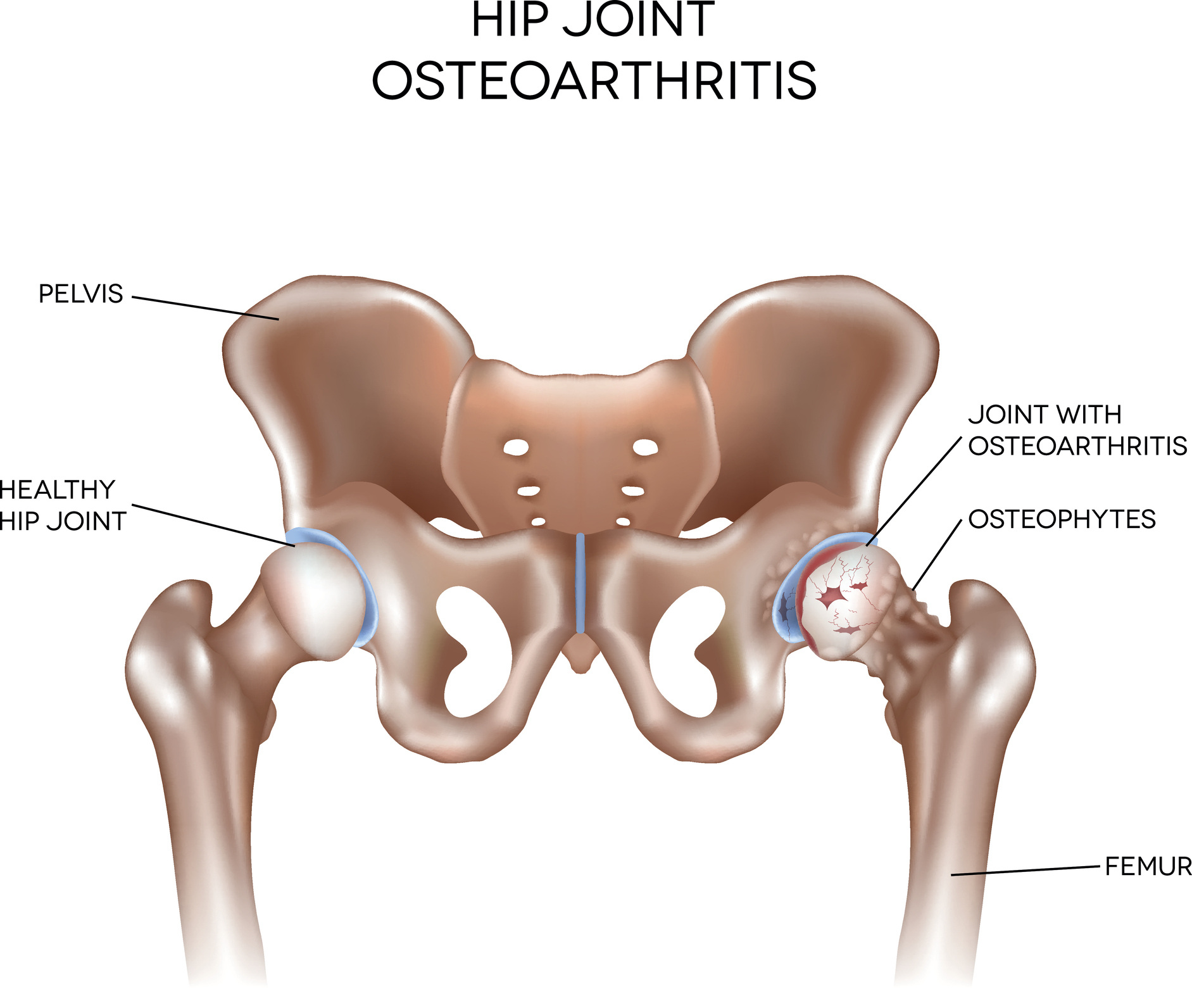
Hip Osteoarthritis (OA)
The hip joint is the largest and one of the most-used weight-bearing joints and is crucial for many activities. The smooth, friction-free movement in a healthy hip is made possible by thin cartilage on both sides of the ball-and-socket joint.
Cartilage should last a lifetime, but it can gradually break down, leading to a degenerative joint disease called osteoarthritis (OA). Factors known to increase the risk of OA include age, previous injury, obesity, genetics, and occupations or sports involving repetitive stress on the joints.
Symptoms of OA typically develop gradually and worsen over time. They can include joint pain, stiffness, swelling, and decreased range of motion. Symptoms may be more pronounced after periods of inactivity or with certain movements, and they can seriously impact quality of life. In more severe cases where conservative treatments have been exhausted, joint replacement surgery may be recommended.
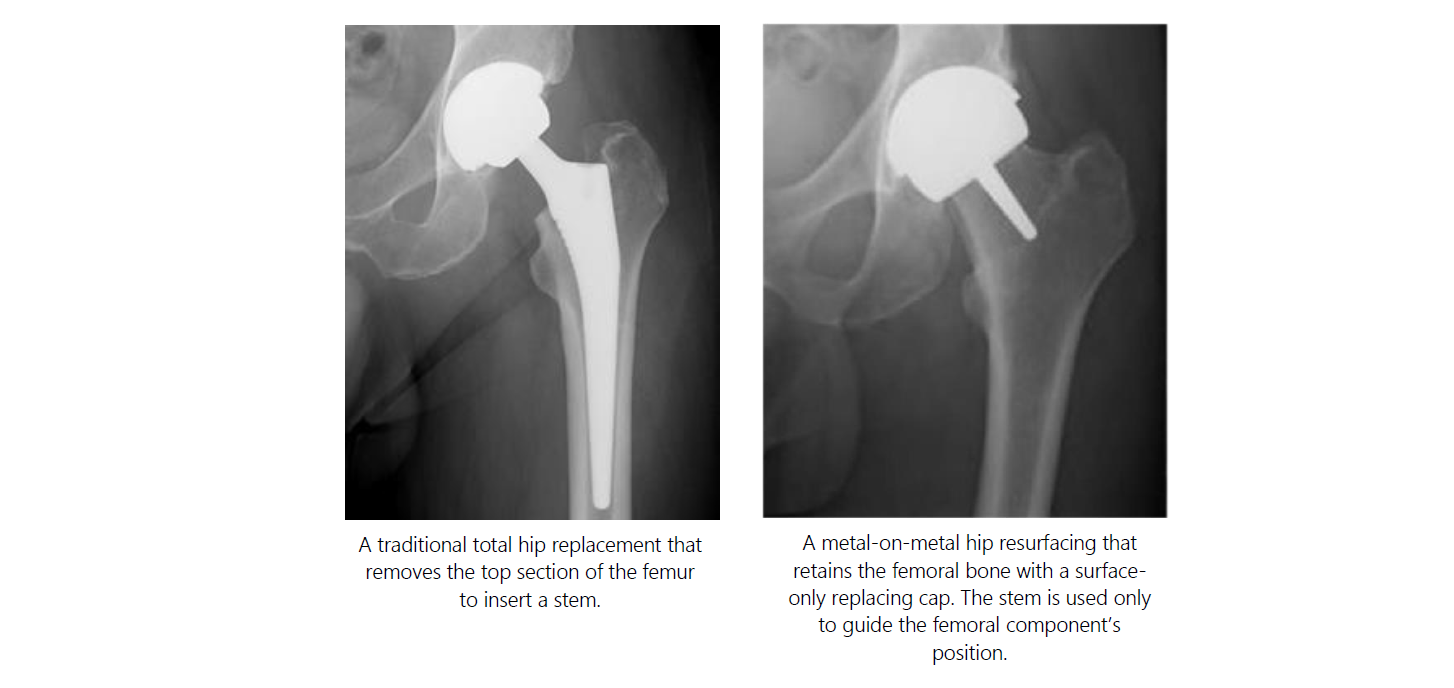
In these cases, total hip replacement (THR) surgery is traditionally prescribed. However, an alternative, more conservative option called hip resurfacing may be considered before a THR.
This brochure will guide you through the benefits of hip resurfacing and why it might be the right choice for you.
As with any surgery, consulting with an orthopaedic surgeon is essential to determining the best course of action based on individual circumstances.
Hip Resurfacing
Hip resurfacing is a surgical procedure designed to address hip OA while preserving more of your natural bone. Unlike traditional total hip replacement surgery, where the entire femoral head is removed, hip resurfacing involves reshaping the damaged surface of the femoral head and capping it with thin-shelled components that have a similar thickness to the removed cartilage. This approach allows for more natural function, greater stability, and a reduced risk of dislocation.
Many patients enjoy decades of improved function and quality of life with a hip resurfacing. Some patients who receive a hip resurfacing may never need a THR. If conversion to a THR is required in later life, the surgery is, in principle, more straightforward than revision of a failed THR.
Benefits of Hip Resurfacing:
Bone Preservation: With hip resurfacing, more of your natural bone is preserved2. This can be advantageous for younger, more active individuals who may require future surgeries, as it provides a larger amount of native bone for potential revision surgeries.
Normal Function: Hip resurfacing allows for a more natural pattern of walking (gait)3,4.
Normal Activity: Expert surgeons agree that they allow their hip resurfacing patients to return to a wider variety of sports and leisure activities without restriction as compared to THR. Patients report a high level of activity including running3,5,6,7,8, and return to activity is commonly earlier in the postoperative recovery phase5,6.
Reduced Risk of Dislocation: The larger femoral head used in hip resurfacing can reduce the risk of dislocation compared to THR and provide greater stability during movement1. This may be particularly beneficial for patients who engage in high-impact activities or have a higher risk of dislocation due to anatomical factors.
Range of Motion: Hip resurfacing can offer excellent stability and a wide range of motion, allowing you to engage in activities you enjoy without discomfort.
Long-Term Durability: When performed on appropriately selected patients, hip resurfacing can provide durable and long-lasting relief from hip pain. The larger bearing surface area and enhanced biomechanics of hip resurfacing may contribute to the longevity of the implant compared to smaller THR components. High levels of activity are maintained for more than 10 years after their operation8.
Younger Patient Population: Hip resurfacing is often considered for younger, more active patients who may have higher demands and expectations for their hip function. By preserving more native bone and offering improved stability, hip resurfacing may more effectively accommodate the lifestyle and activity level of younger patients.
Patient Satisfaction: Many patients who undergo hip resurfacing report high levels of satisfaction with the procedure and an improved quality of life.
If further surgery is required in the future to implant a total hip replacement, the femoral part of the revision surgery is technically the same as a primary (first-time) hip replacement because the femoral bone was retained.
The ADEPT® Hip Resurfacing
The concept of hip resurfacing is not new. Because of its benefits, many notable surgeons in the past have attempted to resurface the hip, including Sir John Charnley, who is recognised for innovating modern THR.
With improved implant designs, enhanced surgical techniques, surgeon experience, and careful patient selection criteria, long-term data, and research show that hip resurfacing has become an ideal option for many people who would traditionally be prescribed a THR.
The ADEPT® Hip Resurfacing, developed by pioneers in the field, has been clinically used since 2004 with high success rates. In the UK, it receives an ODEP 15A rating9, indicating quality and extensive clinical data. It offers excellent outcomes and long-term prospects, especially for young, active patients who might alternatively be prescribed a THR10. In Australia, over 95% of patients haven't needed revision surgery 10 years post-operation, and 93.5% at 15 years10. More information is available at www.matortho.com.

What Are the Risks?
Your consultant will discuss surgery risks and benefits, including any specific to your case. The risks of hip replacement include delayed healing, nerve, or blood vessel damage, swelling, and deep vein thrombosis. General risks reported in registries include bone fracture, dislocation, implant fracture, metal ion release, infection, loosening, and pain. Pre-surgery tests assess bone quality, but if unsuitable during surgery, the surgeon may opt against hip resurfacing.
Your surgeon will be happy to discuss any of this with you.
Available Information
Established hip resurfacing devices such as the ADEPT® have been in clinical use for 20 years or more, and there is a good amount of clinical data on their performance. Here are some helpful links to explore the risks associated with receiving a hip implant:
- The UK Patient National Joint Registry Guidance for Patients: https://www.njrcentre.org.uk/patients/
- The Annual Report: https://reports.njrcentre.org.uk/
- The Orthopaedic Data Evaluation Panel (ODEP): https://www.odep.org.uk/
- The Australian and New Zealand National Joint Registries Report: https://aoanjrr.sahmri.com/annual-reports-2023
Preparing for Surgery
Before your operation, you'll undergo various tests and procedures, including X-rays, blood tests, and an electrocardiogram (ECG). A physiotherapist may fit you for crutches and educate you on postoperative care. To prepare, complete paperwork, ask questions, and make necessary arrangements and changes at home. Avoid anti-inflammatory medications, refrain from eating and drinking before surgery, and don't shave the operation area yourself. Your healthcare team will offer additional advice tailored to your needs.
The Surgical Procedure
The hospital stay typically ranges from one to three days, based on individual needs and standard hospital protocols. Hip resurfacing is commonly performed under spinal or general anaesthesia. During the procedure, a single incision measuring 8-20 cm is made on the outer hip.
Damaged cartilage and bone are removed, and the hip ball and socket are resurfaced with metal components. Closure is done with stitches or clips, followed by dressing application. The duration of the operation, usually around one hour, depends on complexity and potential complications.
After Surgery
After returning to your room, the nursing team will continue monitoring your recovery. Once the anaesthesia wears off, you can eat and drink. Simple exercises in bed will aid your hip joint's movement and muscle strengthening. Within a day of surgery, you'll start walking with a frame. By days two and three, the physiotherapist will assist you in transitioning to crutches or a walking stick and provide additional exercises.
Returning Home
After your healthcare team approves your recovery and you can safely navigate stairs, you'll go home. Arrange for someone to drive you, as you won't be able to. Gradually increase activity and keep up with exercise. Walking is encouraged; go as far as you are comfortable daily.
Expect swelling, bruising, and stiffness, which are normal after surgery. Avoid prolonged sitting to minimise discomfort. If you notice any symptoms or decline in hip function compared to before surgery, consult your doctor, as it could indicate issues with your hip resurfacing.

Figure 2: iStock.com/Amorn Suriyan
Useful Tips and Information
Your healthcare team will offer guidance during recovery and address any questions about returning to normal activities. Follow these guidelines: avoid bending your hip past 90 degrees, refrain from crossing legs, and avoid twisting on your hip when standing or seated. Wait 4-6 weeks before driving, especially if you are still on pain medication; consult your doctor and car insurance company.
Returning to work typically takes 6-12 weeks, depending on recovery and job type. Stitches are removed about 2 weeks post-surgery; avoid getting the dressing wet until then. Shower instead of bathing for the first two days after stitch removal. Resume sexual activity when ready. Your consultant will assess your progress at 6 weeks, aiming for a return to most daily activities. These are general guidelines; follow personalised advice from your healthcare team.
Up to One Year Post-Surgery
During the first post-operative 6 to 12 months, the bone will integrate with the device. You should discuss returning to leisure and sporting activities, which place a higher demand on the joint replacement with your surgeon, who can offer the most up-to-date advice. During this time, you should protect the joint replacement from any unreasonable stresses.
Levels of function and satisfaction will vary between patients, and you should be aware that the hip resurfacing device may not restore function to the level expected with a normal, healthy joint for some people.

Figure 3: iStock.com/GlobalStock
Exercises
Exercise plays a crucial part in the aftercare and recovery following your operation, and your physiotherapist will guide you on what you should be doing. It is important to make sure you only do suitable exercises at the right time during your recovery.
Look Forward to Getting Back to What You love!
With two decades of clinical use, the evidence demonstrates that the ADEPT® Hip Resurfacing is the best treatment option for many patients. As a company, we continue to develop and invest in this procedure to ensure resurfacing is available for everyone. We are both passionate and focused on improving the lives of all patients who receive one of our devices.
Your surgeon, healthcare team, friends, and family want you to get back to doing the things you love. Your recovery in many ways is down to your preparation, mental attitude, willpower, and determination. Patients who use our device include famous athletes who have returned to Olympic level activity, such as surfers, marathon runners, and rugby players. We hope that this can inspire you to get back to your normal.
We wish you the best with your surgery and hope to keep you Forever Active!
Please Note
All information provided in this document is written for guidance purposes only. Your medical team will tailor your treatment to your individual needs.
References
1. National Joint Registry 19th Annual Report, 2022 www.njrreports.org.uk.
2. Lombardi AV et al. Clin Orthop Relat Res. 2011; 469(6): 1547-53.
3. Barrack RL et al. Clin Orthop Relat Res. 2013; 471: 3803–3813.
4. Aqil A et al. Int Orthop. 2013; 37 (5): 795-801.
5 Van Der Straeten C and De Smet KA. Hip Int. 2016; 26 (1):1-7.
6. Girard J. Orthop Traumatol Surg Res. 2015; 101(1 Suppl): S25-9
7. Plate JF et al. J Long Term Eff Med Implants. 2013; 23(4):315-21.
8. Haddad FS et al. Bone Joint J. 2015; 97-B:617–22.
9. ODEP rating for bearing sizes 48-58mm. Latest ODEP ratings can be found at www.odep.org.uk
10. Australian Orthopaedic Association National Joint Replacement Registry. Hip, Knee & Shoulder Arthroplasty: 2021
Annual Report. Adelaide: AOA. 2021. https://aoanjrr.sahmri.com .